Information
Our 48 credit point Master of Perioperative Medicine M6033, has been designed with an increased emphasis on a progression through the units, culminating in a capstone project which aims to consolidate all prior learning and pull together all learning objectives.
This project provides the opportunity for individual creativity as per Monash Graduate Attributes and the Australian Qualifications Framework (level 9).
To recap, the learning objectives for the overall Master of Perioperative Medicine course are:
- Provide clinicians with information to care for the growing complexity of surgical patients.
- Provide a greater understanding of the importance and functioning of the pre-admission clinic.
- Equip the perioperative physician to risk stratify and optimise care of the patient in the perioperative period.
- Collaboratively manage the patient in the perioperative period, in particular the perioperative management of patients with chronic medical illnesses and other organ dysfunction.
- Equip the perioperative physician with the managerial skills to lead a multidisciplinary perioperative management team.
- Equip the perioperative physician with basic research skills to further perioperative medicine research.
To increase flexibility the capstone units are split into 2 units, each worth 6 credit points requiring 10-12 hours of study each week (on average).
The unit breakdown is as follows:
- POM5105 contains 6 learning modules and allows time for working on the capstone project. Go to POM5105
- POM5106 allows you to devote time to completion and submission of the capstone project. Go to POM5106Each of these units are worth 6 credit points each. They can be done concurrently with a similar workload to units POM5101, POM5102 and POM5103.
- For increased flexibility, they can also be done in separate semesters BUT POM5106 must be completed in your last semester of enrollment.
These two new units are offered to all students enrolled in the Master of Perioperative Medicine M6033, and to those students enrolled in course M6027 who have chosen the course variation to complete the course via this pathway.
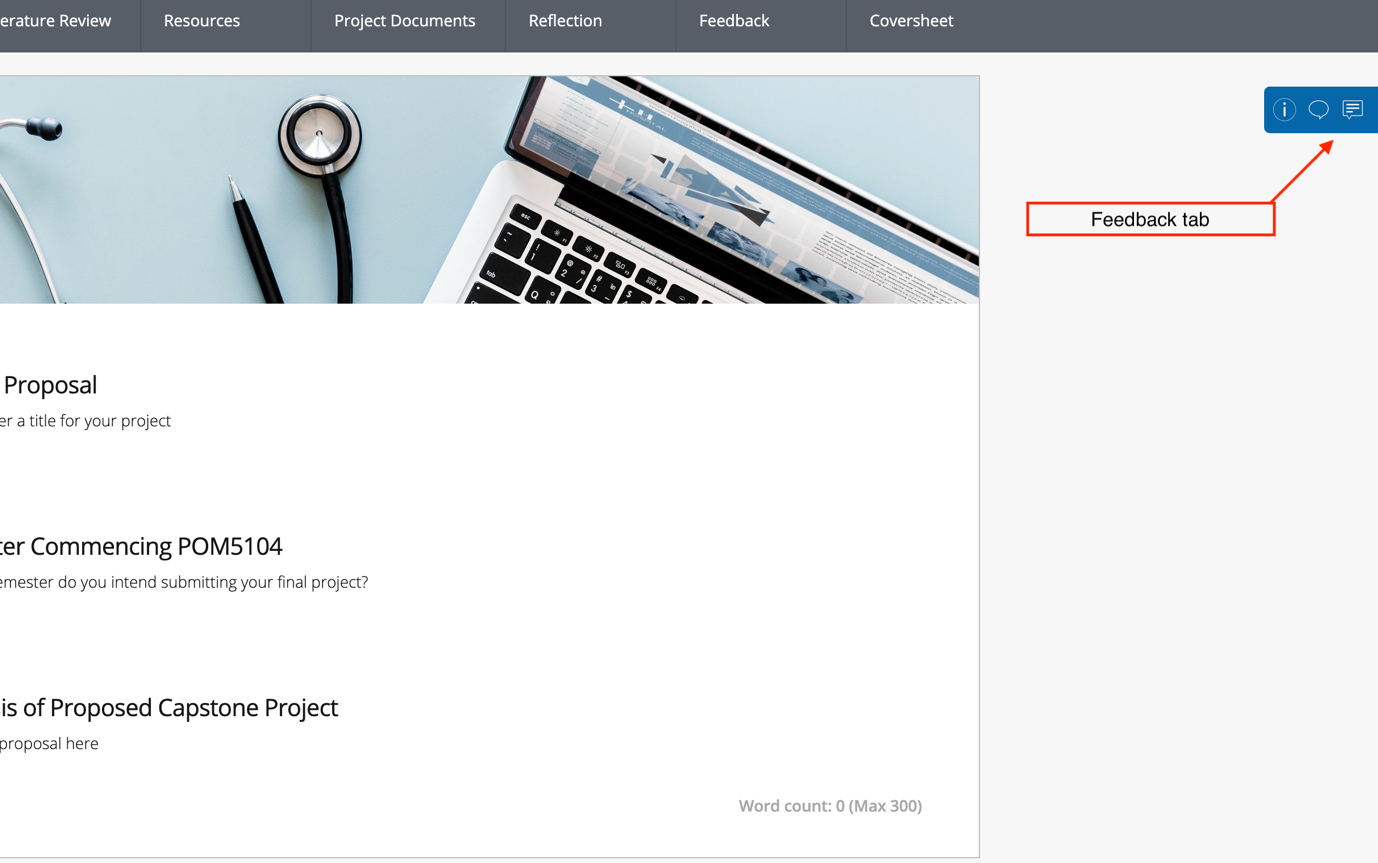
To aid planning and preparing for the capstone project we have introduced a learning journey platform called the PebblePad. We encourage all students to start thinking about, and working on, their capstone project as early as possible. Within the PebblePad platform you will be able to access an online workbook to help guide you through your project - from proposal to completion and submission. Completion of this workbook will comprise part of the assessment tasks of the two new units, POM5105 and 5106. More detail on this, including instructional videos, is provided to all enrolled Master of Perioperative Medicine students at the beginning of first semester.
Capstone Project
The final capstone project will be a 6,000 word report, or equivalent. Students will be encouraged to plan their capstone as they progress through the course. The initial proposal submission will be part of the assessment (5%) and will need to be completed by week 2 of unit POM5105.
Proposal submission will be via the PebblePad workbook. It will be possible for the proposal to be submitted earlier, even before enrolling in unit POM5106, with the credits for assessment saved for the unit.
The capstone must relate to the candidate’s own practice e.g. plans for implementing change at their local hospital or in their practice.
Capstone Unit Framework

There will possibly be the option to work in pairs or groups subject to the appropriate approval of a suitable proposal.
This will be a much more challenging area than any of our current assessments but there will be comprehensive guidelines and suggestions. Suggestions for appropriate projects will include (but are not limited to):
- Audit – meeting SQUIRE 2.0 criteria.
- Design of an iSAP – with full story board preparation and maybe preliminary materials (examples will be provided from other courses).
- Design, construction and proposed implementation of educational material or information for patients/staff, etc. – possible areas to address - communication around race, gender, indigenous patients, refugees, developing world, mental illness.
- A proposal for change at the candidate’s institution – including evidence, presentation to management, costings and initial implementation plan, e.g. change relating to patient blood management, cervical spine trauma, etc.
- Proposal for introduction of a perioperative medicine service at the candidate’s institution – with similar criteria to above.
Capstone Projects for the past Master of Perioperative Medicine students
- Development of a protocol for the care of #NOF patient.
- Development/extension of a perioperative medicine service for a hospital or a subgroup of patients (elderly, complex urology, hip fractures etc).
- Development of a geriatrician led perioperative service in a regional hospital.
- The association between post-anaesthetic care unit length of stay and post-operative deterioration.
- PCA and its effect on postoperative outcomes in older cohort of patients undergoing elective orthopaedic surgeries.
- Proposal to introduce point of care (viscoelastic) testing at a tertiary hospital.
- Prehabilitation for older patients having surgery.
- PAC training module for junior doctors.
- iSAP on complex geriatric patient concentrating on frailty and surgical outcomes, and advance care planning.
- The development of an ERAS/perioperative medicine pathway for major urology patients.
- Audit of time to surgery of patients with diabetic foot ulcers.
- The development of an ERAS/perioperative medicine pathway for major urology patients.
- Implementation of an Enhanced Recovery After Surgery (ERAS) Protocol for Cardiac Surgery.
- Factors associated with postoperative blood transfusions following renal transplantation.
- Anaesthetist led information sessions for obstetric patients on epidural analgesia during labour.
- ISAP - Management of a Jefferson's fracture in the context of dementia and newly diagnosed progressive supranuclear palsy.
- Assessing the risk factor for perioperative AKI and analysing the validity of simple postoperative AKI risk (SPARK) classification before non-cardiac surgery.
- Fit testing of N95 respirator for anaesthetist and anaesthetic nurses.
- Perioperative pathway for patients having elective hip and knee arthroplasty surgery.
- Perioperative management of the palliative patient undergoing surgery.
- What are the benefits of pre-assessment clinics?.
- Analysis of Patient Selection for Rapid COVID-19 (SARS-CoV-2) Testing
- Neuromuscular Monitoring Project.
Capstone Project Podcasts
Dr Lana Vestarkis is an Anaesthetist at Sunshine Coast University Hospital. For her Master of Perioperative Medicine Capstone Project, Lana worked with her colleague Dr Anna Pietzsch to attempt to rationalise preoperative blood testing in the elective surgical setting. Their project is not only having a major impact in their health network but has gone on to win a national prize. Lana and Anna discuss their project, including the challenges faced and the lessons learned when trying to bring about change.
Capstone Project: Choosing Wisely - Redesigning the Pre-anaesthetic Process in a Rural Practice
Dr Sarah Wilmot is a GP Anaesthetist in rural Victoria. For her Master of Perioperative Medicine Capstone Project, Sarah redesigned the pre-anaesthetic process in her practice in an effort to improve patient experience. She discusses her project, including the challenges she faced and the lessons learned when trying to bring about change. Note: this podcast was recorded earlier this year. At the time, Sarah had been recently diagnosed with a terminal illness. Despite feeling unwell she was keen to share her project with a wider audience. Tragically Sarah passed away last month. This conversation is shared in memory of Dr Sarah Wilmott and her dedication to the best care of her patients.